Penn Research Identifies Brain Network that Controls Spread of Seizures
A flurry of coordinated activity in a brain-spanning network of neurons may sound like the formation of a brilliant new idea, but it is actually the description of a seizure. Understanding why and how this synchronization spreads would be a critical tool in treating severe epilepsy.
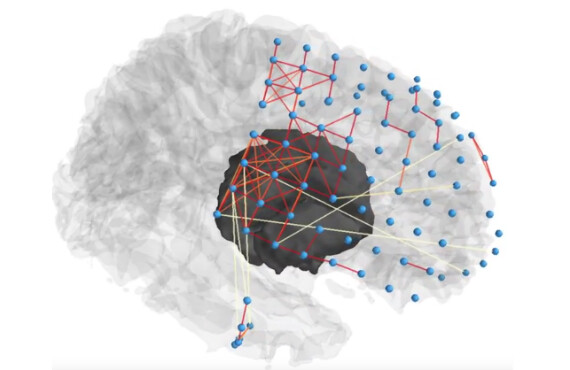
In a study published in Neuron, an interdisciplinary team of University of Pennsylvania researchers has identified a new explanation for this phenomenon. Using a computer model based on direct brain recordings from epilepsy patients, they are the first to show the existence of a network of neural regions that can push or pull on the synchronization of the regions directly involved in a seizure.
With further study, this regulatory network could be a more effective target for epilepsy therapies, including implantable stimulation devices that would help quiet a localized seizure before it spreads throughout the brain.
[youtube]6fIVu0GZsvc[/youtube]
The study was led by Danielle Bassett, Eduardo D. Glandt Faculty Fellow and associate professor in the Department of Bioengineering in the School of Engineering and Applied Science, Brian Litt, professor of neurology and neurosurgery in Penn’s Perelman School of Medicine and of bioengineering in Engineering and director of the Penn Epilepsy Center, and Ankit Khambhati, Bassett’s postdoctoral fellow and a recent graduate of the Litt Lab. Medicine’s Kathryn Davis, assistant professor of neurology, and Timothy Lucas, assistant professor of neurosurgery and co-director of the Penn Center for Neuroengineering and Therapeutics, also contributed to the work
As a network scientist, Bassett studies how the interconnections between members of a group influence the behavior of the whole. Looking at epilepsy through that lens, she, Litt, and Khambhati developed a computer model of seizure networks based on brain recordings from Penn’s epilepsy patients. An earlier study using that model showed that the algorithms in the model can predict where in the brain a seizure will originate and which groups of neurons it will likely spread to as it grows.
In their new study, the researchers aimed to understand how focal seizures, which are limited to only a part of the brain, become general seizures, which spread throughout the brain and are therefore more dangerous and debilitating.
“For people with epilepsy, there are a number of areas of the brain that are really broken—that’s the seizure-generating network,” Bassett said. “Our hypothesis was that there is a separate regulatory network that is usually able to quiet the seizure, and for people whose seizures generalize, that regulatory network is also broken.”
“No one has really talked about this regulatory network before,” she said.
In their new study, the researchers have shown that this second network acts on the one directly involved in the seizure, influencing whether the pathological synchronization remains confined to a local area or spreads across the brain.
“As a dysfunction in the ability of the brain to regulate the communication of information between brain regions,” Khambhati said, “seizures can be thought of as a traffic flow problem. If, on one hand, all the traffic lights at an intersection are green, drivers from all directions attempt to cross at once, in complete synchrony, leading to a jam. On the other hand, if all the lights are red, drivers remain stationary and information ceases to flow. The most efficient road network should coordinate traffic flow where different groups of drivers are moving and stopped at different times.”
To study how seizure networks synchronize and desynchronize, the researchers added a new dimension to their simulation. Using a technique known as “virtual cortical resection,” they could simulate the surgical removal of different sections of the brain. Resection of regions implicated in the seizure network is a last-ditch treatment for severe epilepsy; using virtual cortical resection, the researchers could test the impact of targeting the regulatory network instead.
“Our virtual cortical resection technique,” Khambhati said, “enables us to map the locations of synchronizing, or green-light, and desynchronizing, or red-light, brain regions that facilitate the flow of information. Intuitively, our results showed that seizures are more likely to spread in brain networks with a weaker capacity to limit traffic flow via desynchronizing brain regions.”
“In engineering terms,” Bassett said, “we think this regulatory network has what is known as a ‘push-pull regulatory control.’ There are some regions of the regulatory network that can push the seizure network into a less active state, or pull it out of that state.”
This “push-pull” mechanism appears to work in a manner similar to other biological processes that maintain homeostasis, such as the regulation of heart rate or body temperature, but the researchers are the first to show this kind of regulatory network for epilepsy.
Identifying which regions are which in a patient’s regulatory network could guide new treatment options, such as implantable stimulation devices that would bolster the nodes that help quiet seizure activity, or laser surgery to eliminate the nodes that promote it.
“Our team’s method offers an exciting way to simulate the effect of different therapeutic interventions on patients and predict outcome and side effects,” Litt said. “Functional simulations of this type have tremendous potential to guide new treatments for a variety of neurological disorders and diseases that affect other parts of the body as well.”
This National Institutes of Health recently awarded the group a $4.5 million grant to continue with their epilepsy research.
The study was supported by the National Institutes of Health through awards R01-NS063039, 1U24 NS63930-01A1, Neil and Barbara Smit, the Citizens United for Research in Epilepsy, the Mirowski Foundation, the John D. and Catherine T. MacArthur Foundation, the Alfred P. Sloan Foundation, the Army Research Laboratory and the Army Research Office through contract numbers W911NF-10-2-0022 and W911NF-14-1-0679, the National Institute of Health (2-R01-DC-009209-11, 1R01HD086888-01, R01-MH107235, R01-MH107703, and R21-M MH-106799), the Office of Naval Research, and the National Science Foundation (BCS-1441502, CAREER PHY-1554488, and BCS-1631550). The content is solely the responsibility of the authors and does not necessarily represent the official views of any of the funding agencies.