Penn Professors Lead Call for Ethical Framework for New 'Mind Control' Technologies
As interventions for mental illnesses and neurological disorders are becoming increasingly powerful, an interdisciplinary group of researchers from the University of Pennsylvania, American University and Duke University are calling for new safeguards to guide treatments and protect patients.
In a perspective article published in the journal Nature Human Behavior, they argue that these interventions should now be thought of as a form of “mind control.” As such, neuroscientists, clinicians and bioethicists should begin looking toward the engineering discipline of control theory as a way to better understand the relationship between brain physiology and mental states.
Control theory describes how dynamic, interconnected systems, such as the ones that govern an airplane or nuclear power plant, work together to safely and efficiently deliver a desired outcome. Applied to the brain, it should guide treatments such that patients gain or maintain control over their own mental states as much as possible.
The Penn authors are John Medaglia, research assistant professor in the School of Arts & Science’s Department of Psychology, and Danielle S. Bassett, Eduardo D. Glandt Faculty Fellow and associate professor in the School of Engineering and Applied Science’s departments of Bioengineering and of Electrical and Systems Engineering. They collaborated with Perry Zurn, assistant professor in the Department of Philosophy at American University, and Walter Sinnott-Armstrong, Chauncey Stillman Professor in Practical Ethics in the Department of Philosophy and the Kenan Institute for Ethics at Duke University.
“While we don’t believe,” Bassett said, “that the science-fiction idea of mind control, totally overriding a person’s autonomy, will ever be possible, new brain-focused therapies are becoming more specific, targeted and effective at manipulating individuals’ mental states. As these techniques and technologies mature, we need systems in place to make sure they are applied such that they maximize beneficial effects and minimize unwanted side effects."
“Most treatments we employ already have overlapping effects,” Medaglia said. “Drugs for Parkinson’s disease boost motor function but can also make patients more impulsive. As drugs and other interventions get more powerful, we want to guide them so patients maintain as much autonomy as possible. And, in situations where unwanted side effects are unavoidable, patients should be fully informed what those changes in their mental states might mean for them.”
As advances in molecular biology and chemical engineering are increasing the precision of pharmaceuticals, even more spatially-targeted technologies are emerging. New noninvasive treatments send electrical currents or magnetic waves through the scalp, altering the ability of neurons in a targeted region to fire. Surgical interventions are even more precise; they include implanted electrodes that are designed to quell seizures before they spread, or stimulate the recall of memories after a traumatic brain injury.
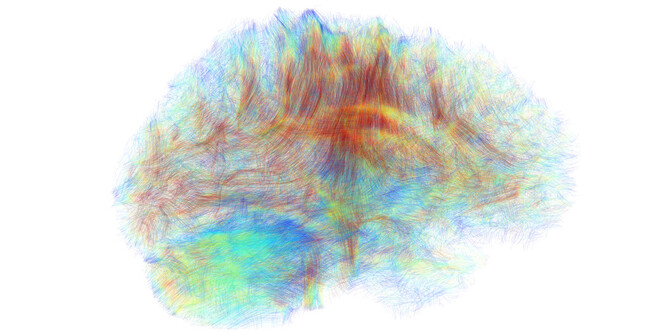
Research into the brain’s “wiring” — how neurons are physically connected in networks that span disparate parts of the brain — and how this wiring relates to changing mental states has enabled principles from control theory to be applied to neuroscience. For example, a recent study by Bassett and colleagues shows how changes in brain wiring from childhood through adolescence leads to greater executive function, or the ability to consciously control one’s thoughts and attention.
While insights from network science and control theory may support new treatments for conditions like obsessive compulsive disorder and traumatic brain injury, the researchers argue that clinicians and bioethicists must be involved in the earliest stages of their development. As the positive effects of treatments become more profound, so do their potential side effects.
“New methods of controlling mental states will provide greater precision in treatments,” Sinnott-Armstrong said, “and we thus need to think hard about the ensuing ethical issues regarding autonomy, privacy, equality and enhancement.”
"Pairing network neuroscience and control theory promises to provide greater precision in clinical care,” Zurn said. “As this work develops from an ethically-informed perspective, it will prompt better mental health-care policies and a stronger cultural appreciation of the body-mind continuum."
The authors see their article itself as emblematic of the trajectory this work must take: neuroscientists, bioethicists, philosophers and physicians coming together to prepare for the opportunities and challenges these new technologies will introduce.