Penn Med Team Reports on Study of First 59 Leukemia Patients Who Received Personalized Cellular Therapy
Three and a half years after beginning a clinical trial which demonstrated the first successful and sustained use of genetically engineered T cells to fight leukemia, a research team from the Perelman School of Medicine at the University of Pennsylvania and the Children’s Hospital of Philadelphia will today announce the latest results of studies involving both adults and children with advanced blood cancers that have failed to respond to standard therapies. The findings from the first 59 patients who received this investigational, personalized cellular therapy, known as CTL019, will be presented during the American Society of Hematology’s Annual Meeting and Exposition in New Orleans.
wo of the first three chronic lymphocytic leukemia (CLL) patients who participated in the study, which started in the summer of 2010, remain in remission, with tests revealing reprogrammed cells still circulating in their bodies, on guard to combat tumor cells that may reappear in the future. Additional highlights of the new research results include an 89 percent complete response rate among adult and pediatric patients with acute lymphoblastic leukemia (ALL).
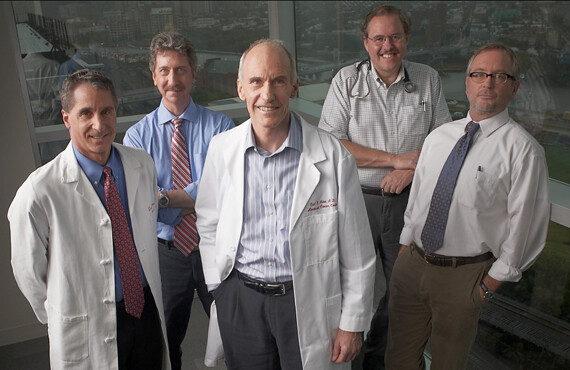
“In a very short time, we’ve learned so much about how CTL019 works and how powerful it can be,” said the research team’s leader, Carl H. June, MD, Richard W. Vague Professor in Immunotherapy in the department of Pathology and Laboratory Medicine and director of Translational Research in Penn’s Abramson Cancer Center. “Our findings show that the human immune system and these modified ‘hunter’ cells are working together to attack tumors in an entirely new way.”
The research team, which includes investigators who treat patients at both the Hospital of the University of Pennsylvania and the Children’s Hospital of Philadelphia, will announce findings from trials of three different groups of patients:
- 15 of 32 adult patients with CLL (47 percent) responded to the therapy, with seven of those experiencing a complete remission of their disease. Results of both the completed pilot study of 14 CLL patients (Abstract #4162) and results thus far of the first 18 patients in a Phase II, dose-optimization trial (Abstract #873) will be presented.
- 19 of 22 pediatric patients with ALL (86 percent) experienced complete remissions. The first pediatric patient treated with the protocol, who is now 8 years old, remains in remission 20 months later. Five patients have relapsed, including one whose tests revealed new tumor cells that do not express the protein targeted by the reprogrammed cells. (Abstract #67)
- All five of the first adult ALL patients treated thus far experienced complete remissions, the longest of which continues six months after treatment. One patient subsequently underwent a bone marrow transplant and remains in remission. One patient relapsed after three months with disease that also tested negative for the engineered cell target. (Abstract #67)
Building a Cancer-Killing CAR
The investigational treatment pioneered by the Penn team begins by removing patients' T cells via an apheresis process similar to blood donation, then reprogramming them in Penn’s cell and vaccine production facility with a gene transfer technique using a lentivirus vector. The newly built T cells target tumor cells using an antibody-like protein, called a chimeric antigen receptor (CAR), which is expressed on the surface of the T cells and designed to bind to a protein called CD19, which is found on the surface of the cancerous B cells associated with both CLL and ALL.
The modified cells are then infused back into the patient's body following lymphodepleting chemotherapy. In the body, these “hunter” T cells both multiply and attack. A signaling domain built into the CAR promotes rapid growth of these cells, building an army of tumor-killing cells that tests reveal can grow to more than 10,000 new cells for each single engineered cell patients receive. Cells in the patient that do not express CD19 are left untouched by the modified T cells, which limits the prolonged, systemic side effects typically experienced during traditional cancer therapies that harm healthy tissue.
Click here to view the full release.