Blood Cancers Develop When Immune Cell DNA Editing Enzyme Hits Off-target Spots in the Genome, Penn Animal Study Finds
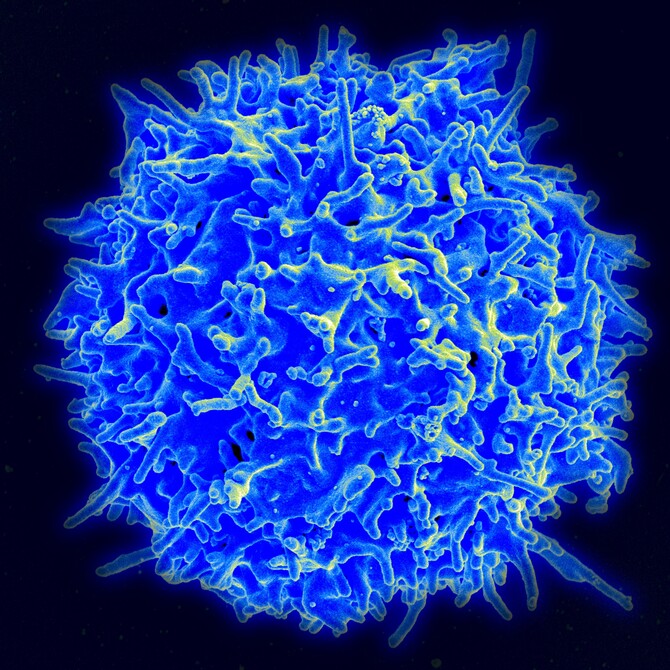
Sometimes when the immune system makes small mistakes, the body amplifies its response in a big way: Editing errors in the DNA of developing T and B cells can cause blood cancers. Now, researchers from the Perelman School of Medicine, University of Pennsylvania have shown that when the enzyme key to cutting and pasting segments of DNA hits so-called “off-target” spots on a chromosome, the development of immune cells can lead to cancer in animal models. Knowing the exact nature of these editing errors will be helpful in designing therapeutic enzymes based on these molecular scissors. The Penn team’s findings appear online this week in Cell Reports ahead of the print issue.
V(D)J recombinase, the editing enzyme that generates specific receptors on the surface of immune cells that match foreign invaders, collectively called antigens, can miss its target from time to time. The lab of senior author David Roth, MD, PhD, chair of the Department of Pathology and Laboratory Medicine, has been working out the cancer-related intricacies of V(D)J recombinase for the last two decades. “Knowledge of the exact nature of these off-target errors could lead to the development of safer versions of tools for genetic engineering,” Roth said.
V(D)J recombinase works only during the early stages of immune cell maturation. From this stage in the bone marrow, the diverse array of antibodies and cell-surface receptors found on immune B cells and T cells, respectively, are made to counteract all the foreign invaders the human body encounters.
Breaks in DNA strands associated with V(D)J cutting are normally repaired with high fidelity by finely tuned molecular machinery. Previous studies from the Roth lab showed that V(D)J recombinase (consisting of the RAG1 and RAG2 proteins) normally sends a break in DNA down the correct repair path by preventing access to other, inappropriate repair mechanisms. This shepherding process can be disabled if the “C” terminus of the RAG2 protein subunit is removed. This causes genomic instability in developing immune cells and, in the absence of a working tumor suppressor protein such as p53, an aggressive form of lymphoma develops in mice.
Genome wide analysis of lymphomas of the thymus in these mice with the truncated Rag2 protein revealed a surprise: numerous off-target DNA rearrangements, causing deletions, noted Roth. Previous work had suggested that a different mistake -- chromosome translocations, or swaps between two chromosomes -- might underlie the development of lymphoma in these mice, but whole genome sequencing revealed deletions as the main drivers of these cancers.
These rearrangements affected several known and suspected oncogenes and tumor suppressor genes, including Notch1, Pten, Ikzf1, Jak1, Phlda1, Trat1, and Agpat9.